Introduction
Table of Contents
Micrococcus luteus, often simply referred to as M. luteus, is a Gram-positive, spherical bacterium belonging to the genus Micrococcus. This bacterium is commonly found in various environments, including soil, dust, water, and on the human skin. Micrococcus species are known for their distinctive yellow or golden pigmentation, and M. luteus is no exception, as its name “luteus” is derived from the Latin word for “yellow.”
Here is a brief introduction to some key aspects of Micrococcus luteus:
- Morphology: M. luteus is typically characterized by its small, round cells (coccoid shape) that occur singly, in pairs, or in irregular clusters. The cells are non-motile and lack flagella. They are usually around 1 to 2 micrometers in diameter.
- Coloration: As mentioned earlier, M. luteus is known for its distinctive yellow or golden color. This color results from the production of pigments, particularly carotenoids, which serve various functions, including protecting the bacterium from harmful UV radiation.
- Habitat: It is a ubiquitous bacterium, and it can be found in a wide range of environments. It is commonly found in soil, where it plays a role in nutrient cycling. It is also present on human skin, where it is considered part of the normal skin microbiota.
- Metabolism: M. luteus is aerobic, meaning it requires oxygen for its metabolism. It is a chemoorganotrophic bacterium, which means it obtains energy by oxidizing organic compounds. It can metabolize a variety of substrates, including sugars and amino acids.
- Role in Biotechnology: Micrococcus luteus has been studied for its potential applications in biotechnology. It produces enzymes such as catalase and amylase, which are of interest in various industrial processes. Additionally, its pigments, particularly the carotenoids, have potential commercial value.
- Non-pathogenic: It is generally considered non-pathogenic to humans. It is not a common cause of infections and is not associated with disease. In fact, it is often used as a model organism in laboratory studies due to its relatively simple genetics and ease of cultivation.
- Antibiotic Production: Some strains of M. luteus are known to produce antibiotics, which can inhibit the growth of other bacteria. These antibiotics may play a role in competition for resources in their natural habitats.
Morphology
The morphology of Micrococcus luteus is characterized by distinctive features that make it easily identifiable under a microscope. Here are the key aspects of the morphology of M. luteus:

- Cell Shape: It is a spherical bacterium, which means it has a coccoid or cocci shape. Cocci are round or oval cells, and M. luteus cells typically appear as small, spherical entities.
- Cell Size: The size of M. luteus cells can vary slightly, but they are generally quite small. The typical diameter of M. luteus cells ranges from approximately 0.5 to 3 micrometers, with an average size of around 1 to 2 micrometers.
- Arrangement: Its cells can occur singly, in pairs (diplococci), in tetrads (groups of four), or in irregular clusters. The arrangement of cells can vary depending on their growth conditions and nutrient availability.
- Gram Staining: Micrococcus luteus is classified as a Gram-positive bacterium. This means that its cell wall structure contains a thick layer of peptidoglycan, which retains the crystal violet stain used in the Gram staining procedure. As a result, Micrococcus luteus cells appear purple or violet when subjected to Gram staining.
- Coloration: One of the distinguishing features of M. luteus is its yellow or golden color. This pigmentation is due to the production of pigments, including carotenoids, which give the bacterium its characteristic hue. Carotenoids also serve a protective role by absorbing harmful UV radiation.
- Motility: Its cells are non-motile, meaning they do not possess flagella or other structures for active movement. They rely on passive diffusion for nutrient uptake and dispersion.
- Capsule: Some strains of Micrococcus luteus may produce a slimy capsule around their cell wall. This capsule can be involved in protection, adherence to surfaces, or evasion of the host immune system.
Pathogenicity
Micrococcus luteus is generally considered to be a non-pathogenic bacterium to humans. It is commonly found in the environment, including soil, dust, water, and on human skin, where it is part of the normal skin microbiota. In most cases, it does not cause infections or disease in healthy individuals. Instead, it is regarded as a commensal bacterium, meaning it coexists harmlessly with the host.
Here are some reasons why Micrococcus luteus is typically not pathogenic:
- Lack of Virulence Factors: Micrococcus luteus lacks many of the virulence factors commonly associated with pathogenic bacteria, such as toxins, adhesins, and invasive enzymes. These factors are necessary for bacteria to cause diseases.
- Non-invasive: It is not an invasive bacterium, meaning it does not have the ability to penetrate tissues or enter the bloodstream, which is a characteristic of many pathogenic bacteria.
- Low Pathogenic Potential: Even if introduced into the body through a wound or injury, Micrococcus luteus is unlikely to cause an infection because it is not well-adapted to survival and proliferation in the human body.
- Immunocompetence: Healthy individuals with functioning immune systems are generally able to keep M. luteus and other non-pathogenic bacteria in check, preventing them from causing disease.
However, it’s important to note that in rare cases, Micrococcus luteus has been reported as an opportunistic pathogen. This means that it can potentially cause infections in individuals with compromised immune systems, such as those with severe underlying medical conditions, immunosuppression, or open wounds. In such cases, Micrococcus luteus may be involved in opportunistic infections, such as wound infections or bloodstream infections.
While Micrococcus luteus is not a primary pathogen like some well-known disease-causing bacteria, it is always important to maintain good hygiene and proper wound care to minimize the risk of any potential infections, including those caused by opportunistic bacteria. If someone with a weakened immune system or other risk factors develops an infection suspected to be caused by M. luteus, appropriate medical attention and treatment should be sought.
Lab Diagnosis
The laboratory diagnosis of Micrococcus luteus involves several microbiological techniques and tests to identify and characterize the bacterium. Here is a step-by-step guide to diagnosing Micrococcus luteus in a laboratory setting:

- Sample Collection: Obtain a sample suspected to contain M. luteus. This could be a clinical specimen (e.g., a wound swab) or an environmental sample (e.g., soil, water).
- Isolation and Cultivation: Inoculate the sample onto a suitable culture medium. Micrococcus luteus can grow on a variety of media, including nutrient agar or trypticase soy agar. Incubate the agar plates at a suitable temperature (usually around 30-37°C) for 24-48 hours.
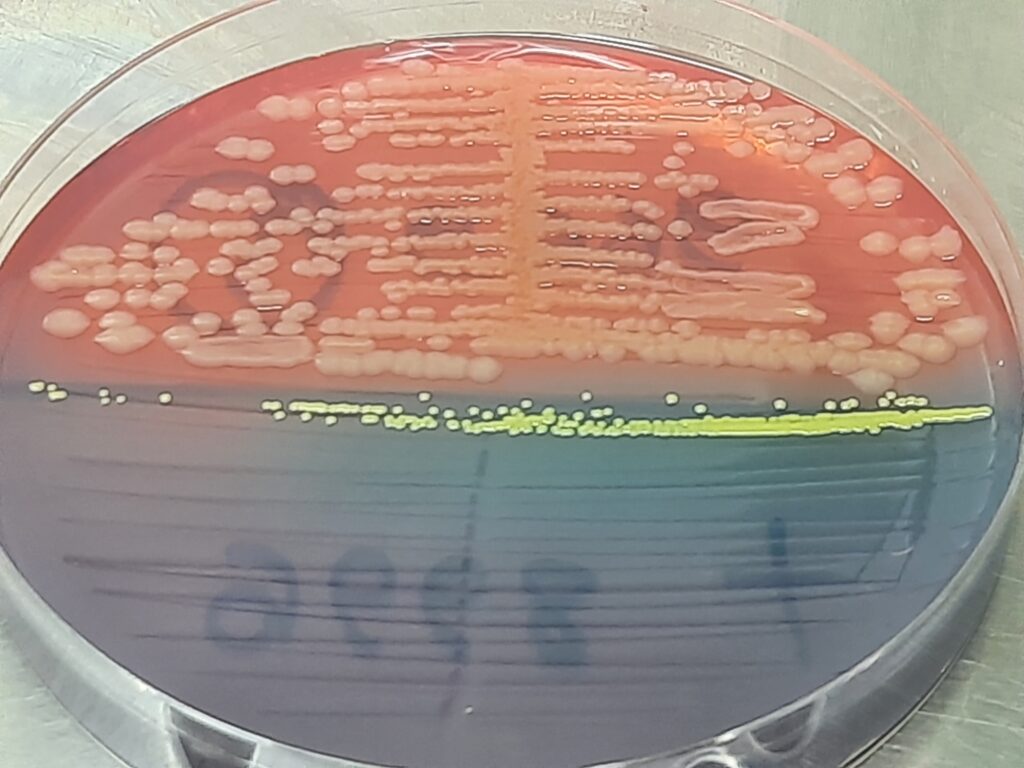
- Colonial Morphology: Examine the agar plates for the presence of colonies that are typical of Micrococcus luteus. Characteristics of M. luteus colonies include:
- Yellow or golden coloration (due to carotenoid pigments).
- Circular and convex shape.
- Smooth and shiny texture.
- Gram Staining: Perform a Gram stain on a representative colony. M. luteus is Gram-positive, so its cells will appear purple or violet under the microscope.
- Microscopic Examination: Examine the stained smear of the colony under a microscope. Micrococcus luteus cells are typically spherical (cocci) and occur singly, in pairs (diplococci), or in clusters.
- Biochemical Tests: Perform a series of biochemical tests to confirm the identity of the isolated bacterium as Micrococcus luteus. Common biochemical tests include:
- Catalase Test: M. luteus is catalase-positive, meaning it produces the enzyme catalase, which generates bubbles when hydrogen peroxide is added to a colony.
- Coagulase Test: It is coagulase-negative, meaning it does not produce the enzyme coagulase.
- Oxidase Test: Micrococcus luteus is oxidase-negative, meaning it does not produce the enzyme oxidase.
- Sugar Fermentation: Test for the ability of the bacterium to ferment various sugars, such as glucose and lactose.
- Antibiotic Susceptibility Testing: Perform antibiotic susceptibility testing to determine the sensitivity of the isolated Micrococcus luteus strain to various antibiotics. This helps guide treatment if the bacterium is associated with an infection.
- Molecular Identification (Optional): For a more definitive identification, molecular techniques like polymerase chain reaction (PCR) and DNA sequencing can be used to target specific genes, such as the 16S rRNA gene, for species-level identification.
- Storage and Documentation: If needed, store the isolated strain for further analysis or reference. Document the results of all tests and observations for future reference.
Treatment
Micrococcus luteus is generally considered a non-pathogenic bacterium in healthy individuals and is not typically associated with infections that require specific treatment. It is commonly found in the environment, including on human skin, where it is part of the normal skin microbiota. However, in rare cases, Micrococcus luteus can cause opportunistic infections, especially in individuals with weakened immune systems or underlying medical conditions. In such cases, appropriate treatment may be necessary.
Treatment of infections caused by M. luteus or other opportunistic pathogens generally involves the following steps:
- Identification and Diagnosis: Confirm the presence of Micrococcus luteus or another causative organism through appropriate laboratory testing, including culture and identification of the bacterium.
- Antibiotic Sensitivity Testing: Perform antibiotic susceptibility testing to determine which antibiotics are effective against the specific strain of M. luteuscausing the infection. Micrococcus luteus is typically susceptible to a range of antibiotics.
- Antibiotic Therapy: Administer antibiotics that have been found to be effective against the strain of Micrococcus luteus causing the infection. Commonly used antibiotics may include penicillin, ampicillin, vancomycin, or other antibiotics, depending on the results of sensitivity testing.
- Wound Care: If the infection is localized, such as a skin wound infection, appropriate wound care is essential. This may include cleaning and disinfection of the wound, debridement (removal of dead tissue), and dressing changes.
- Supportive Care: In cases where infections have spread or caused complications, supportive care may be necessary. This could include hydration, pain management, and addressing any underlying medical conditions.
- Monitoring: Regularly monitor the patient’s progress and response to treatment. Adjust the antibiotic therapy if necessary based on the clinical response and any changes in antibiotic sensitivity patterns.
- Preventive Measures: In healthcare settings, infection control practices, including proper hand hygiene, sterilization of medical equipment, and isolation precautions, can help prevent the transmission of opportunistic pathogens like Micrococcus luteus to vulnerable patients.
It’s important to note that M. luteus infections are rare, and most individuals with healthy immune systems do not develop infections from this bacterium. The majority of Micrococcus luteus strains are harmless and can even be beneficial in some cases, such as in biotechnological applications. Treatment is typically reserved for cases where the bacterium is causing clinically significant infections in immunocompromised individuals.
Prevention
Preventing infections and the proliferation of Micrococcus luteus, which is generally non-pathogenic but can become opportunistic in certain conditions, primarily involves good hygiene and infection control practices. Here are some preventive measures to consider:
- Hand Hygiene: Proper handwashing is one of the most effective ways to prevent the spread of Micrococcus luteus and other potentially harmful microorganisms. Encourage regular handwashing with soap and warm water, especially after using the restroom, before eating, and after being in contact with potentially contaminated surfaces.
- Environmental Hygiene: Maintain cleanliness in the environment, particularly in healthcare settings, by regularly cleaning and disinfecting surfaces and medical equipment. Proper sterilization procedures should be followed for reusable medical devices.
- Infection Control in Healthcare: In healthcare settings, adhere to infection control guidelines and practices. This includes the use of personal protective equipment (PPE), such as gloves and gowns, and implementing isolation precautions when necessary to prevent the transmission of opportunistic pathogens.
- Wound Care: Properly clean and dress wounds to prevent infections. This is particularly important for individuals with compromised immune systems or open wounds.
- Antibiotic Stewardship: Inappropriate use of antibiotics can lead to antibiotic resistance. Prescribe antibiotics only when necessary and based on sensitivity testing results to avoid the development of antibiotic-resistant strains of M. luteus.
- Immunization: Ensure that individuals who are at risk due to underlying medical conditions or immunosuppression are up to date with relevant vaccinations to reduce the risk of infections.
- Personal Hygiene: Encourage individuals to maintain good personal hygiene, including regular bathing and cleaning of the skin. While Micrococcus luteus is a normal component of the skin microbiota, keeping the skin clean can help minimize the risk of infection.
- Food Safety: Practice safe food handling and preparation techniques to prevent foodborne illnesses. Although M. luteus is not typically associated with foodborne infections, general food safety practices are important.
- Respiratory Hygiene: In healthcare settings and during respiratory illness outbreaks, promote respiratory hygiene practices, such as covering the mouth and nose when coughing or sneezing, and provide proper respiratory etiquette education.
- Infection Prevention Education: Educate healthcare workers, patients, and the general public about infection prevention measures and the importance of good hygiene practices.
- Regular Health Check-ups: For individuals with compromised immune systems or chronic medical conditions, regular health check-ups and monitoring are essential to identify and address any potential infections promptly.
Keynotes
Here are some key points or notes on Micrococcus luteus:
- Classification: It is a Gram-positive, spherical bacterium belonging to the genus Micrococcus.
- Morphology: It has a coccoid or cocci shape, with small, round cells that can occur singly, in pairs, or in clusters. The cells are typically around 1 to 2 micrometers in diameter.
- Coloration: Micrococcus luteus is known for its yellow or golden color, which results from the production of pigments, including carotenoids.
- Habitat: It is commonly found in various environments, including soil, dust, water, and on human skin, where it is part of the normal skin microbiota.
- Metabolism: It is aerobic, chemoorganotrophic, and non-motile. It obtains energy by oxidizing organic compounds.
- Pathogenicity: It is generally considered non-pathogenic to healthy individuals but can cause opportunistic infections in immunocompromised individuals.
- Laboratory Diagnosis: Diagnosis involves culture and isolation on appropriate media, Gram staining, biochemical tests (catalase test, oxidase test), and antibiotic sensitivity testing.
- Treatment: Infections caused by M. luteus are rare but may be treated with antibiotics based on sensitivity testing if necessary. Good wound care is also important.
- Prevention: Preventive measures include good hand hygiene, environmental cleanliness, infection control in healthcare settings, proper wound care, and appropriate antibiotic use.
- Role in Biotechnology: Some strains of Micrococcus luteus are used in biotechnological applications due to their ability to produce enzymes and pigments.
- Commensal Bacterium: In most cases, M. luteus is considered a commensal bacterium, coexisting harmlessly with the host.
- Antibiotic Production: Certain strains of Micrococcus luteus are known to produce antibiotics that inhibit the growth of other bacteria.
Further Readings
- Microbiology Textbooks: Consider referring to microbiology textbooks, such as “Microbiology: An Introduction” by Gerard J. Tortora, Berdell R. Funke, and Christine L. Case or “Brock Biology of Microorganisms” by Michael T. Madigan, John M. Martinko, and Kelly S. Bender. These textbooks often provide comprehensive information on various microorganisms, including Micrococcus species.
- Scientific Journals: Search for articles on Micrococcus luteus in scientific journals. You can use academic databases like PubMed, Google Scholar, or your institution’s library resources to access peer-reviewed research papers and studies. Look for articles on its genetics, physiology, metabolism, and applications in biotechnology.
- Microbiology Research Articles: Explore research articles specific to Micrococcus luteus. Topics may include its role in environmental microbiology, antibiotic production, and its use as a model organism in laboratory research.
- Clinical Microbiology Texts: If you’re interested in the clinical aspects of Micrococcus luteus, consult clinical microbiology textbooks like “Murray & Nadel’s Textbook of Respiratory Medicine” or “Clinical Microbiology Procedures Handbook.” These sources may discuss the bacterium’s relevance in clinical settings.
- Review Articles: Review articles often provide comprehensive summaries of the current state of knowledge about specific microorganisms. Search for review articles on Micrococcus luteus to get a well-rounded understanding of its biology and applications.
- Microbial Physiology Journals: Journals specializing in microbial physiology, such as the “Journal of Bacteriology,” may feature research on various aspects of Micrococcus luteus, including its metabolic pathways and growth characteristics.
- Biotechnology Resources: If you’re interested in Micrococcus luteus’ applications in biotechnology, explore resources related to industrial microbiology and bioprocessing. You may find articles and books discussing its role in enzyme production, pigment synthesis, or other biotechnological processes.
