Introduction
Table of Contents
Nasal swab culture and sensitivity is a diagnostic laboratory test used to identify and determine the antibiotic sensitivity of microorganisms present in the nasal passages. It is a valuable tool in the diagnosis and management of various respiratory infections, particularly those caused by bacteria. This procedure helps healthcare providers identify the specific bacteria causing an infection and determine the most effective antibiotic treatment.
Here’s how the process typically works:
- Nasal Swab Collection: A healthcare professional will take a sterile swab and gently insert it into the patient’s nostril. The swab is then rotated against the nasal lining to collect a sample of mucus and any potentially present microorganisms.
- Transport to the Laboratory: After collection, the swab is placed in a specialized transport medium that maintains the viability of the collected microorganisms during transportation to the laboratory.
- Inoculation and Incubation: In the laboratory, the nasal swab sample is streaked onto specific culture media that support the growth of bacteria. The media provide a controlled environment for the microorganisms to multiply.
- Identification: After an appropriate incubation period, the bacteria colonies that have grown on the culture media are examined and identified by their characteristic appearance, such as shape, color, and growth pattern. Modern laboratories may also use automated identification systems for more accurate and rapid results.
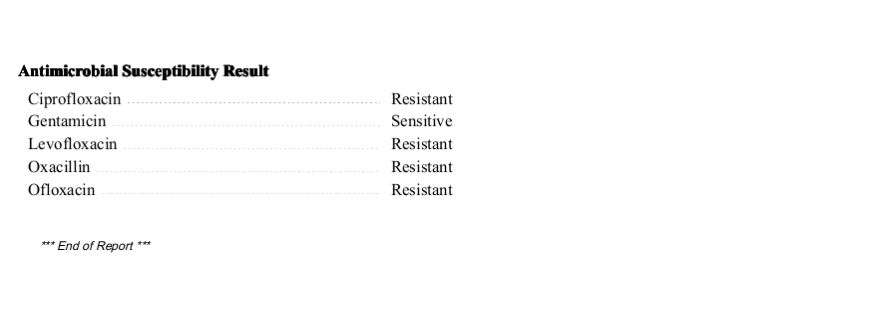
- Antibiotic Sensitivity Testing: Once the bacteria are identified, they are subjected to antibiotic sensitivity testing. This process involves placing small discs containing different antibiotics onto the culture media. If the bacteria are susceptible to a particular antibiotic, there will be an area of reduced growth around the antibiotic disc (called a “zone of inhibition”).
- Interpretation and Reporting: The laboratory personnel interpret the results based on the growth patterns and zone of inhibition around the antibiotic discs. A report is generated and sent to the healthcare provider, indicating the specific bacteria identified and the antibiotics to which it is sensitive. This information helps the doctor choose the most appropriate antibiotic for effective treatment.
Nasal swab culture and sensitivity is commonly used to diagnose and manage infections such as bacterial sinusitis, nasal carriage of MRSA (Methicillin-resistant Staphylococcus aureus), and other respiratory tract infections. It is important to note that this test is specific to bacterial infections and cannot identify viral infections.
As with any medical test, accurate and timely diagnosis is crucial for effective treatment and patient care. Nasal swab culture and sensitivity play a vital role in guiding healthcare providers towards the most suitable antibiotic therapy, helping to avoid unnecessary or ineffective treatments and contributing to better patient outcomes.
Report

Clinical Significance
Nasal swab culture and sensitivity have significant clinical importance in the diagnosis and management of various respiratory infections. Here are some of the key clinical significances of this diagnostic test:
- Identifying Bacterial Infections: Nasal swab culture and sensitivity are particularly useful in identifying bacterial infections of the respiratory tract. By isolating and identifying the specific bacteria causing the infection, healthcare providers can tailor treatment to target the causative pathogen accurately.
- Antibiotic Selection: The sensitivity testing performed on the cultured bacteria helps determine which antibiotics will be most effective in treating the infection. It provides critical information on the susceptibility of the bacteria to different antibiotics, allowing physicians to prescribe the most appropriate and targeted therapy.
- Guiding Empirical Therapy: In some cases, physicians may initiate treatment with empirical antibiotics (broad-spectrum antibiotics) before culture results are available. Nasal swab culture and sensitivity results can guide adjustments to the initial antibiotic regimen, ensuring that patients receive the most suitable antibiotic for their specific infection.
- Preventing Antibiotic Resistance: The test helps to limit the use of broad-spectrum antibiotics, which can contribute to antibiotic resistance. By identifying the specific bacteria and their sensitivities, healthcare providers can use narrow-spectrum antibiotics whenever possible, reducing the risk of antibiotic resistance development.
- Monitoring Outbreaks: Nasal swab culture and sensitivity can be instrumental in monitoring and controlling outbreaks of bacterial infections. In settings such as hospitals, nursing homes, or schools, identifying the bacteria responsible for an outbreak helps implement appropriate infection control measures to prevent further transmission.
- Differentiating Bacterial from Viral Infections: Respiratory tract infections can have bacterial or viral origins, and their symptoms often overlap. Nasal swab culture and sensitivity can help differentiate between the two types of infections, preventing unnecessary antibiotic use for viral infections, which are not responsive to antibiotics.
- Tracking Antimicrobial Resistance Patterns: By analyzing the sensitivity patterns of different bacteria, healthcare authorities can track the emergence of antibiotic-resistant strains. This information is crucial for formulating antibiotic policies and promoting rational antibiotic use.
- Assessing Treatment Response: In cases of chronic or persistent respiratory infections, repeat nasal swab culture and sensitivity can be performed to assess the effectiveness of the chosen antibiotic treatment. It helps identify whether the initial antibiotic therapy is eradicating the infection or if a change in treatment is necessary.
Common Pathogens
Nasal swab culture can identify a wide range of microorganisms that may colonize or infect the nasal passages. The most common pathogens detected in nasal swab cultures include:
- Staphylococcus aureus: Both Methicillin-Sensitive Staphylococcus aureus (MSSA) and Methicillin-Resistant Staphylococcus aureus (MRSA) can be identified. MRSA is particularly concerning as it is resistant to many common antibiotics.
- Streptococcus pneumoniae: A leading cause of bacterial pneumonia, sinusitis, and middle ear infections.
- Haemophilus influenzae: A common cause of respiratory infections, including sinusitis and otitis media.
- Moraxella catarrhalis: Another bacterium associated with respiratory tract infections, particularly in children and the elderly.
- Streptococcus pyogenes (Group A Streptococcus): A pathogen responsible for strep throat and other respiratory infections.
- Neisseria meningitidis: Although more commonly associated with meningitis, it can also be found colonizing the nasal passages.
- Corynebacterium species: Some species of Corynebacterium are part of the normal nasal flora, but certain strains can cause infections.
- Pseudomonas aeruginosa: While commonly associated with infections in hospitalized patients, it can also be found in the nasal passages of healthy individuals.
- Klebsiella pneumoniae: Another bacterium often associated with hospital-acquired infections, but it can also be present in the nasal passages.
- Escherichia coli: Normally found in the intestines, some strains can cause respiratory infections when present in the nasal passages.
It’s important to note that the presence of these pathogens in a nasal swab culture does not necessarily indicate an active infection or illness. Some of these bacteria can be part of the normal nasal flora, meaning they reside harmlessly in the nasal passages without causing any problems. The clinical significance of the results depends on the patient’s symptoms, medical history, and other factors.
Moreover, nasal swab culture is not limited to bacterial pathogens. It can also identify other microorganisms like viruses and fungi if the appropriate culture methods are used. However, viral and fungal cultures are less common in routine nasal swab testing and are usually reserved for specific clinical scenarios.
Keynotes
Keynotes on Nasal Swab Culture and Sensitivity:
- Diagnostic Tool: Nasal swab culture and sensitivity is a diagnostic laboratory test used to identify bacterial pathogens in the nasal passages and determine their antibiotic sensitivity.
- Respiratory Infections: It is commonly used to diagnose respiratory tract infections such as sinusitis, bacterial rhinitis, and other upper respiratory infections.
- Swab Collection: A healthcare professional collects a sample by inserting a sterile swab into the patient’s nostril and gently rotating it against the nasal lining to obtain mucus and microorganisms.
- Transport Medium: The swab is placed in a specialized transport medium to maintain the viability of the collected microorganisms during transportation to the laboratory.
- Culture and Incubation: In the laboratory, the swab sample is streaked onto culture media that support bacterial growth. The media are then incubated to allow the bacteria to multiply.
- Bacterial Identification: After incubation, the bacterial colonies that grow on the culture media are identified based on their appearance and characteristics.
- Antibiotic Sensitivity Testing: The identified bacteria are subjected to antibiotic sensitivity testing to determine which antibiotics are most effective against them.
- Personalized Treatment: The results guide healthcare providers in selecting the most appropriate and targeted antibiotic therapy for the patient’s infection.
- Preventing Antibiotic Resistance: By identifying antibiotic-resistant bacteria, the test helps in promoting rational antibiotic use and reducing the risk of antibiotic resistance development.
- Differentiating Bacterial and Viral Infections: Nasal swab culture and sensitivity can help distinguish between bacterial and viral respiratory infections, aiding in avoiding unnecessary antibiotic prescriptions for viral infections.
- Monitoring Outbreaks: The test is valuable in monitoring and controlling outbreaks of bacterial infections in various settings.
- Follow-Up Testing: In some cases, repeat nasal swab culture and sensitivity may be performed to assess treatment response and adjust therapy if necessary.
- Patient Education: Patients should be educated about the importance of proper sample collection and compliance with prescribed antibiotics to ensure effective treatment.
- Limitations: The test only identifies bacterial pathogens and is not effective for viral or fungal infections.
- Laboratory Turnaround Time: Results may take a day or longer to be available, and in cases of urgent infections, empirical antibiotic treatment may be initiated before results are obtained.
- Interpretation: The interpretation of results should be done by trained laboratory personnel and healthcare providers who can make appropriate clinical decisions based on the findings.
Further Readings
- “Diagnostic Value of Nasal Swabs in the Detection of Methicillin-Resistant Staphylococcus aureus in Different Patient Groups” by Göksel Şener, Serap Süzük, Nida Kılıçaslan, et al. (2015) – This study explores the diagnostic value of nasal swabs in detecting MRSA in different patient groups, providing insights into the clinical significance of nasal swab culture in identifying specific pathogens.
- “Nasal Swab Culture for MRSA Detection: A Diagnostic Accuracy Study” by Y. Glupczynski, A. J. Berhin, L. Bogaerts, et al. (2013) – This study evaluates the diagnostic accuracy of nasal swab culture for MRSA detection, helping to understand the reliability of this diagnostic method.
- “Nasal Carriage of Staphylococcus aureus: Epidemiology, Underlying Mechanisms, and Associated Risks” by F. Wertheim, D. H. Melles, M. C. Vos, et al. (2005) – This review article discusses the epidemiology, underlying mechanisms, and associated risks of nasal carriage of Staphylococcus aureus, shedding light on the importance of nasal swab culture and sensitivity in identifying this pathogen.
- “Comparison of the Sensitivity and Specificity of Three Swab Transport Systems for the Detection of Bacterial Pathogens by Culture in Nasal and Pharyngeal Specimens” by S. J. McDonagh, M. N. Carman, and R. J. G. Chalmers (2014) – This study compares the sensitivity and specificity of different swab transport systems for the detection of bacterial pathogens by culture in nasal and pharyngeal specimens, providing insights into the best practices for sample collection and transport.
- “Antimicrobial Susceptibility Testing: A Review of General Principles and Contemporary Practices” by M. A. Pfaller and D. J. Diekema (2010) – While not specific to nasal swab culture, this review provides valuable information on antimicrobial susceptibility testing principles and practices, which are essential for understanding the interpretation of sensitivity testing results.
- Clinical Microbiology Procedures Handbook, Volume 1: Microbiology Procedures for the Diagnosis of Infectious Diseases (4th Edition) by H. D. Isenberg (Editor) – This comprehensive handbook provides detailed protocols and guidelines for various microbiological diagnostic procedures, including nasal swab culture and sensitivity.
- Laboratory Protocols in Applied Life Sciences – This online resource by Nature Protocols offers a variety of protocols used in laboratory research, including protocols related to bacterial culture and sensitivity testing.
- Centers for Disease Control and Prevention (CDC) – The CDC’s website provides information on diagnostic testing, antimicrobial resistance, and guidelines for the management of infectious diseases, which can be relevant to nasal swab culture and sensitivity.
